Key Takeaways:
-
According to a Black Book Survey, hospital CFOs agree that advancing virtual health (87%), improving patient experiences (73%), and accelerating their transformation of digital financial systems (81%) are top priorities.
-
With an augmented intelligence solution, you see a pure example of what technology married to human intelligence can accomplish in the healthcare business operations field.
-
By taking advantage of advanced technology coupled with targeted human intelligence, we are entering a new phase of proactive revenue generation and collection.
2020 will be remembered as more than just an anomaly. The healthcare industry was faced with an unprecedented public health emergency, and far-reaching financial implications that will continue into 2021, 2022, and beyond. As we reach a new set point for hospital finances following COVID-19, hospital CFOs are collectively committed to maintaining the IT improvement budgets even when other sacrifices may have to be made.
According to the recent Black Book Survey, 100% of the participating healthcare CFOs saw significant revenue decline in 2020 (as much as 30%). But 88% agreed that cuts would be avoided in their digital transformation plans and IT budgets. Top areas for growth include advancing virtual health (87%), improving patient experiences (73%), and a full 81% are focusing on accelerating their transformation of digital financial systems.
5 Augmented Intelligence Solutions That Automate and Transform the Hospital Bottom Line
Hospital CFOs are embracing innovative solutions, including artificial intelligence-guided business systems that are supported by qualified specialists in an augmented intelligence format.
As we look at the five solutions, it’s important to consider that each can be approached as a stand-alone process or as part of a comprehensive business operation. And while some of the solutions are more traditional 3rd party partnerships, others are forward-looking artificial intelligence (AI) automation solutions supported by experienced specialists.
-
Prior Authorizations — Prior authorizations are the least automated business function in all of healthcare with hospitals and providers relying on manual systems and antiquated processes, like phone calls and faxes. With an augmented intelligence solution, you see a pure example of what technology married to human intelligence can accomplish in the healthcare business operations field.
Even though insurance payers can accept electronic prior authorization submissions, the percentage of hospitals participating is minimal (about 21% industry-wide). With an automated AI-driven software supported by specialists ready to handle emergent or complex prior authorizations, hospitals can process them in real-time with follow up monitored 24/7. Patient scheduling can take place almost immediately in most cases with less turnover and case abandonment.
-
Coding — With error rates throughout the industry averaging over five percent, alternative systems that focus on proficiency and proven expertise translate to greater profits.
By engaging in a third-party partnership, hospitals benefit from flexibility and scalability for their coding needs. A further benefit, by utilizing an off-site team, coding can be performed quickly and accurately without the hiring, onboarding, and training issues that accompany FTEs.
- Billing — Successful hospital billing relies on skilled handling and timely completion of the charge entry and payment posting functions. Precise, clean claims processed by trained and certified medical billers delivers maximum reimbursement that flows to the bottom line.
-
AR Optimization through a Comprehensive RCM Platform — Once care has been provided and submitted to the appropriate insurance payers, the large majority is paid. The portion of each visit that’s not covered by insurance is either part of the contracted write-offs or becomes a part of the AR. It’s at this point that an augmented intelligence optimization process would allow a thorough and effective denials management function to take place.
With an AI-driven comprehensive automation process, denials could be worked and resubmitted with specialized billing experts available to handle the complex or problematic issues as they arise. With over 40% of denials never reworked or resubmitted, there is potentially significant revenue capture possible.
-
Insurance Discovery — With coverage in place that isn’t divulged by the patient (known or unknown), money owed often ends up in collections or written off. By utilizing an AI-driven program that taps into massive clearinghouses of insurance information, unidentified insurance is discovered so that claims can be resubmitted and collected.
Using software that utilizes augmented intelligence solutions and machine learning capabilities, along with experienced billing specialists, insurance discovery can be implemented at any time during the patient encounter and billing/collections process.
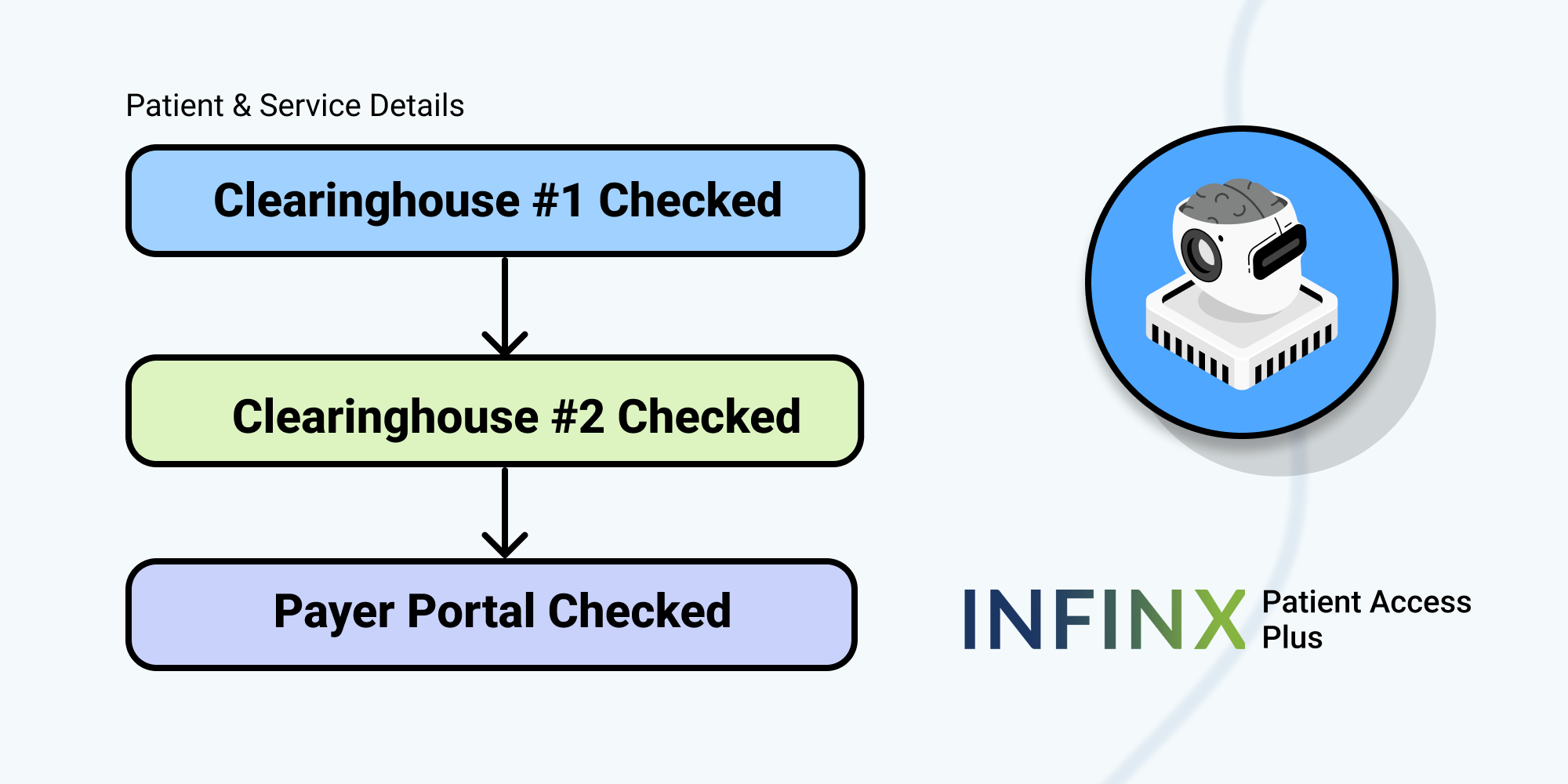
Once the account information is uploaded, the following steps take place:
-
- All undisclosed coverage is deep mined from clearinghouses and insurance payers,
-
- Using probabilistic analytics and machine learning, patient demographic information, insurance profiles, and coverage benefits are identified and verified, and
- Once previously, unidentified coverage is identified, it is then communicated back to revenue cycle management or the EHR/EMR system as the billing continues.
Moving forward following the pandemic, hospitals find themselves with challenges, both financial and care-related. By taking advantage of advanced technology coupled with targeted human intelligence, we are entering a new phase of proactive revenue generation and collection that relies on slow antiquated systems and insurance payers’ imposed limitations and are more resilient and purposeful.
Contact us today to schedule a demo and learn more about augmented intelligence solutions to benefit the hospital bottom line.