In successfully managing the orthopedic payment lifecycle, avoiding denials has long been a time consuming and only moderately successful endeavor. As insurance payers investigate ways to limit their exposure and shift financial responsibility to patients, providers have seen an increase in denials as payment systems change, benefit guidelines shift, and consumer deductibles increase.
With an aging population interested in life-enhancing procedures, such as total joint replacement, orthopedic practices have come more into focus by insurance payers keen on limiting their exposure as elective procedures continue to rise. While you can’t always impact outside forces, let’s look at the top three internal areas of orthopedic denials and some solutions that will alleviate the workflow overload as well as increase reimbursement to the bottom line.
Top 3 Orthopedic Denial Pain Points
When investigating possible improvements for orthopedic revenue challenges, there are three specific areas that are currently being managed manually by over 70% of providers and lend themselves to an automated solution. These three areas have automated opportunities utilizing artificial intelligence (AI) and machine learning, supported by certified specialists to handle emergent requests or outlying issues.
1. Prior Authorization
With 370 healthcare organizations signing on to discuss the burden of prior authorization with a U.S. House of Representatives’ Committee on Small Business recently, prior authorizations (PA) has been identified as the number one administrative burden experienced by providers today. While most PAs are ultimately approved, the process can be time-intensive with each submission often requiring multiple follow up phone calls and faxes, and eventually, appeals.
With an automated and AI-driven software solution that can be fully integrated with your orthopedic EMR/EHR, processes that were once manual can be executed in real-time with little input from your staff including:
- Determining if a PA is required or not and, if so, preparing the appropriate patient demographic and insurance information along with the medical diagnosis, codes, and rationale for the procedure, test, or medication
- Submitting the PA to the insurance payer through their electronic portal
- Monitoring and executing follow up and appeals as appropriate in real-time
- Notifying the scheduling department when the PA has been approved so that preparations can commence
- State-of-the-art reporting and analytics dashboard so that you can obtain full transparency into your prior authorization workflow
2. Insurance Verification and Eligibility Benefits
One of the chief reasons for ortho denials is inaccurate or incomplete insurance verification of patients or eligibility and financial responsibility inaccuracies. This leads to claims denials, rework and appeals, and patient frustration with unexpected billing or canceled procedures.
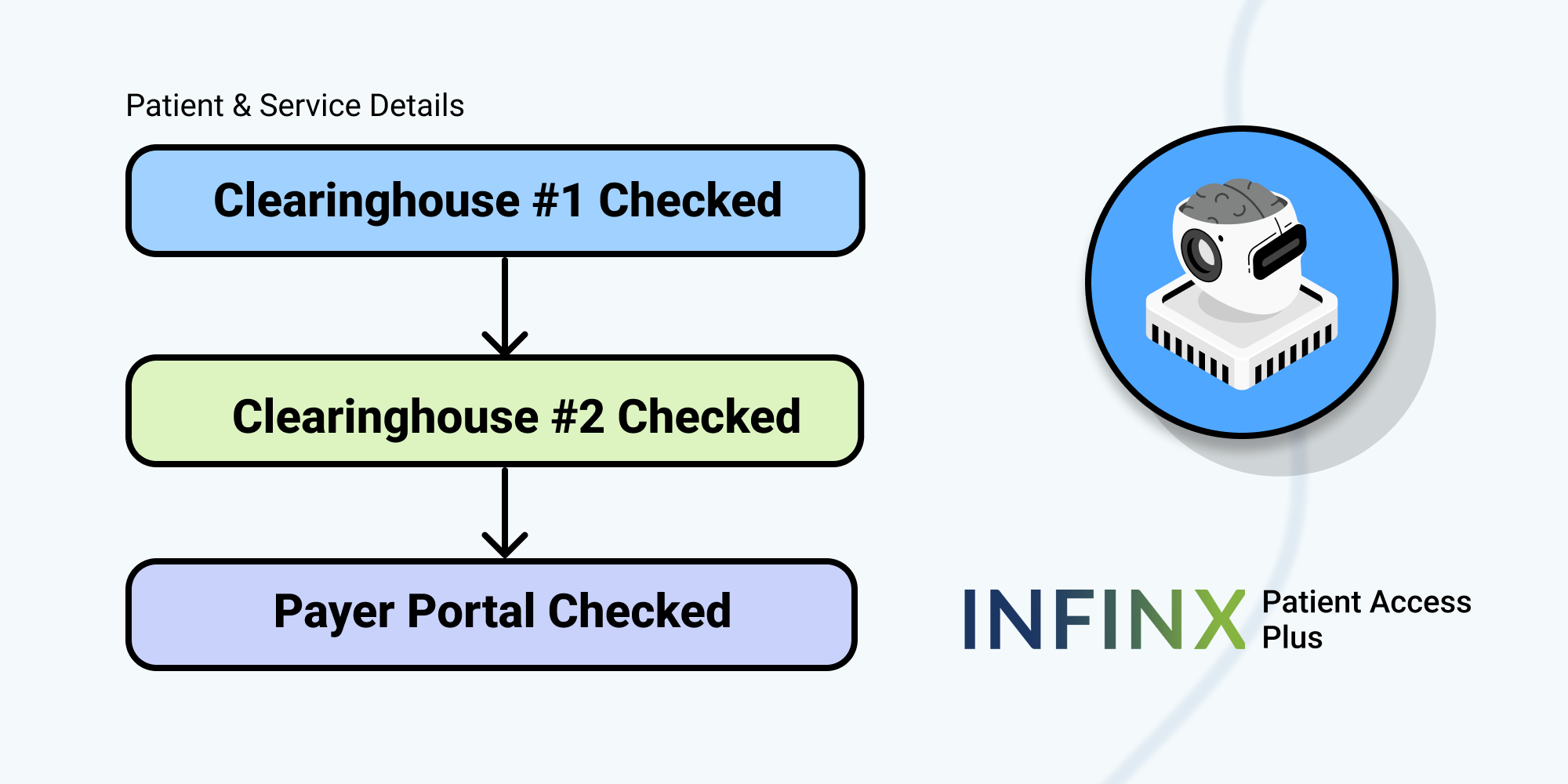
With an integrated and intelligent solution, insurance can be tracked, verified, and available benefits confirmed with precision. This not only helps with revenue cycle management, but the patient’s portion can be prepared and collected prior to the visit or surgery.
3. Denials Management
Another orthopedic revenue challenge is the denials management process and proactively overseeing the Accounts Receivable and Days Outstanding. On average, over 60% of denied claims are abdicated and written off whether due to a lack of time or expertise in the follow-up or appeals process.
Again, through AI-enhancement, the denials management process can be automated in the following ways:
- Predicting and prioritizing recovery and forecasting collectible dollars/timelines
- Determining through predictive analysis the next best course of action for each denial
- Utilizing an integrated system to check EOB status and accuracy, auto-create appeals letters, and resubmission
- Reviewing root causes and solutions to prevent future revenue leakage
- Real-time operation analytics to provide the utmost accuracy and transparency
Orthopedic denials handled manually are very costly to appeal. On average, over 60% of denied claims are recoverable on first appeal, but with a third-party partner offering state-of-the-art automated and AI-driven software and certified specialists to enhance and streamline PAs, insurance verifications, and denials management, your practice can see lost revenue captured and added to your bottom line.
Schedule a demo today and discover how AI-driven software solutions can improve your orthopedic practice revenue.