White Paper
Challenges Preventing Complete Automation for Prior Authorizations

Executive Summary
Although mandated by HIPAA in the early 2000s, electronic automation of the prior authorization workflow has been slow in development and even slower in acceptance and use. In this white paper, we look at several challenges that have precluded prior authorization automation from grabbing a foothold, even more so than other administrative functions, such as insurance verification, benefits eligibility, and patient portion due.
While there are answers and solutions to many of the challenges underway, the bottom line is that total electronic processing, including the use of artificial intelligence (AI) and machine learning capabilities, is an incomplete answer. There needs to be an augmented intelligence solution that marries machine automation and human intellect to realize the goal of efficient prior authorizations fully.

“Artificial Intelligence constitutes a host of computational methods that produce systems that perform tasks normally requiring human intelligence. However, in healthcare a more appropriate term is ‘Augmented Intelligence’, reflecting the enhanced capabilities of human clinical decision-making when coupled with these computational methods and systems.”
–American Medical Association
The Current State of Prior Authorizations
While the original intention set by utilization review, the mechanics of administering prior authorizations has created a cumbersome and unnecessarily awkward process with frequent denials and patient care issues. The recently released “2019 AMA Prior Authorization Physician Survey” notes that over 90% of physicians report that patient care is negatively affected and often results in delays in patient care, including care abandonment.1

To put into even more drastic terms, in the survey, 24% of physicians reported that prior authorization issues led to a serious adverse event for one of their patients. In comparison, a full 16% said that it had led directly to a patient’s hospitalization.
The call for streamlined prior authorization and utilization management reform has been growing louder and more intense over the last several years, so why has little actual movement occurred? Aside from the resistance of insurance payers who stand by their process, there are physical and technical challenges precluding the complete automation of the prior authorization process.

Calls for Change
Whether hospital or practice-based, healthcare providers continue to experience the administrative burdens placed on them by their increasing prior authorization obligations. In the macro sense, the industry continues to absorb an aging population that’s living longer and requires more care, the increasing use of High Deductible Healthcare Plans (HDHP) that transfer additional costs to patients,2 and the perpetual decline in reimbursement due to, among other things, the Protecting Access to Medicare Act of 2014 (PAMA).3
In early 2018, healthcare stakeholders took a more proactive stance in pressuring the Centers for Medicare and Medicaid Services (CMS) and commercial insurance payers to overhaul the prior authorization process, and the efforts have picked up steam in light of the COVID-19 public health emergency. The American Medical Association (AMA), joined by 16 other groups, participated in a joint task force with the sole purpose of developing reform principles to guide a streamlined prior authorization process, and reduce friction.4
Simultaneously, Representative Suzan DelBene proposed “H.R. 3107 – Improving Seniors’ Timely Access to Care Act of 2019,” which seeks to establish numerous prohibitions, requirements, and standards relating to prior authorizations.5
As this proposed bill has made its way through the various committees and procedures that lead up to the final vote, it has been supported by almost every professional and industry association, including the American Health Insurance Plans Association (AHIP), speaking on behalf of insurance payers.
What’s the Financial Impact of Automating the Prior Authorization Process?
According to the “2019 CAQH Index on Conducting Electronic Business Transactions,” 87% of medical practices use a manual system to manage prior authorizations at a system-wide cost of $14.24 per prior authorization. Of that 87%, 51% may use payer website portals to submit and manage or partially manage their prior authorizations. In contrast, the remaining providers use an entirely manual system utilizing telephones and fax machines. Add to that the unworked claims denials experienced from missing or rejected prior authorizations, and the costs to the healthcare industry overall are astronomical.6
Now compare that to the savings and efficiencies available through the use of an automated system, and prior authorizations become much more palatable and manageable to gauge quality and appropriateness of care. On an industry-wide basis, the CAQH Index projects a savings of $12.317 from automated prior authorizations, which would not only achieve the originally intended consequences but also improve the patients’ experience and the provider’s bottom-line
5 Challenges Preventing System-Wide Adoption of Electronic Prior Authorization
In August 2020, CMS announced the “Adopted Standards and Operating Rules”8 where HIPAA required HHS to establish national standards for electronic transactions, defining the adopted standard for prior authorizations as ASC X12N 278 Version 5010 (Phase V of the CAQH CORE findings as the HHS-designated Operating Rule Author).9
While this is a significant step, there remain five industry-wide challenges to fully automated prior authorizations as outlined in the CAQH CORE’s report entitled “Moving Forward: Building Momentum for End-to-End Automation of the Prior Authorization Process”.10
Lack of Data Consistency Throughout the Industry
There is a lack of uniformity between insurance payers in the coding used to communicate status, errors, and next steps. Requirements differ amongst plans and create confusion for providers trying to submit critical information in their requests. In turn, this has been a challenge for automation developers as they try to match intent with payer requirements.

Lack of Mandated Standards for Clinical Documentation and Other Required
Attachments
From payer to payer, there is a shortfall of standardization and uniformity across plans for attachments and clinical documentation resulting from individual payer proclivities. Vendors have found it difficult to create solutions that support HIPAA’s electronic standard for prior authorizations thereby resulting in numerous side steps to reach compliance.
Lack of Clinical and Administrative System Integration
Historically, there has been a lack of integration between EHR/EMR and practice management systems, which has created barriers to an end-to-end automated prior authorization solution. What has been needed, and what Infinx provides, is an automated prior authorization workflow using HL7/API bi-directional integration to automatically connect providers with payers so that it can be determined if a prior authorization is required, or not, and what documentation is needed.

Legislatively, several states have mandated that insurance payers notify providers by phone or USPS mail when there are outliers, such as complex prior authorization approvals and rejections. For instance, in Minnesota, payers must contact providers when a prior authorization is not approved. In Colorado and Rhode Island, providers can speak directly to a qualified medical representative when there is an adverse determination.

Providers are unaware that HIPAA requires health plans to offer the 5010X217 278 Request and Response solution for prior authorizations. While, as stated above, CMS is actively spreading the word about the requirement from HIPAA compelling health plans to accommodate the technology, it will take a proactive push from provider organizations to fully engage their constituency and demand compliance
So, What’s the Solution? A Shifting Paradigm
With an estimated 182 million prior authorization transactions being processed per year, according to the Medical Group Management Association (MGMA),11 it is easy to see where issues are bound to arise related to sheer volume. With that in mind, this fact seems almost inconceivable: prior authorizations are the least automated business function in most practices. While verifying insurance and filing claims is done electronically in many, if not most hospitals, practices, and ancillary or outpatient departments, only 13% of business departments use an automated prior authorization solution.12
Augmented Intelligence – Technology Combined with Human Intelligence Can Solve the Prior Authorization Equation
We hear a lot about AI these days, but what does it mean in terms of solving our most frustrating problems like reducing manual, time-consuming, and repetitious tasks or removing human error from the prior authorization equation?
Augmented intelligence elevates the overall discussion by:
- Accelerating current employee throughput to a higher level
- Augmenting the decision-making process
- Reducing manual processing costs and risks
- Increasing consistency of output
- Continuously self-learning

Explaining How Augmented Intelligence Works
Certainly daunting, explaining how AI works can be formidable; however, this clarification is suitable for our purposes: utilizing a predefined set of algorithms, AI-driven software uses statistical analysis to unlock data insights. It then supports data-driven decisions that improve the timeliness and accuracy of targeted outcomes. AI programming can combine large chunks of data through iterative processing allowing the software to “learn” by memorizing patterns in the data.13
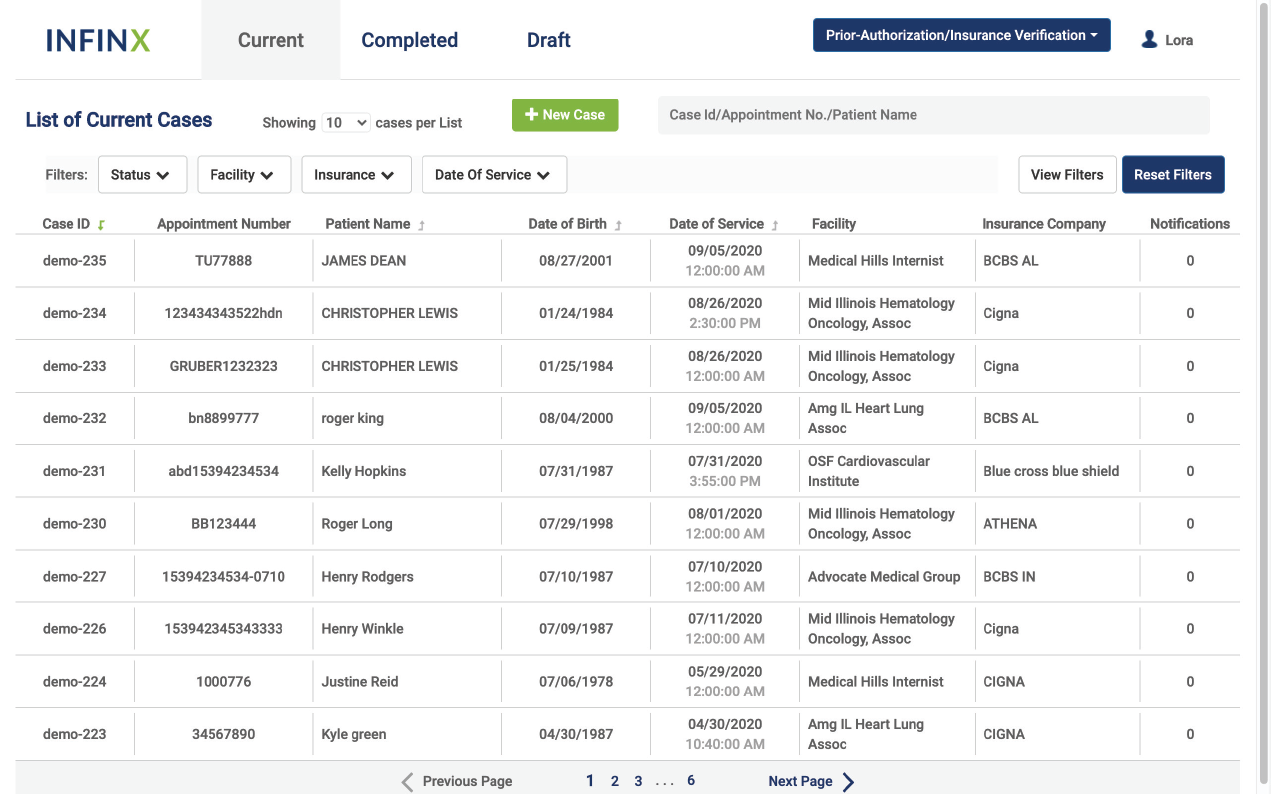
To illustrate through the lens of prior authorizations, AI-driven software would be integrated bi-directionally with a practice or group’s EHR/EMR and billing system being used for client management through cloud-based technology. As a patient’s order is created, tests, procedures, and medications requiring prior authorizations would be electronically identified, a determination would be made as to necessity, provider/facility detail, patient demographics, and test/diagnosis information would be collected. An approval request would then be submitted in real-time to the insurance payer electronically.
Now, as anyone who has worked in healthcare knows, there are invariably outliers and problem examples that come up routinely. This is where a team of highly trained specialists working in tandem with an AI-driven automation solution would handle the exceptions immediately, ensuring swift resolution and submission. Communicating with the practice or group through a secure dashboard portal, their expertise would also be beneficial during any follow-up, or rejection handling that may be required.
Ensuring Up-to-the-Minute Accuracy
To electronically determine the parameters of the prior authorizations and route the request to the appropriate insurance payer portal, AI-driven software with machine learning capabilities would access continually updated insurance information clearinghouses storing thousands of insurance groups and plans, each with their unique guidelines and requirements.
Prior authorization approvals that once took several hours to several days or weeks can now be accomplished in virtually real-time with a 99% accuracy rate, with the outlier-focused team accessing the same up-to-theminute information. With augmented intelligence, you have full end-to-end prior authorization coverage, which is unachievable prior authorization solutions on the market today.
A Comprehensive and Secure Cloud-Based Solution
The Infinx Prior Authorization Software solution creates a seamless and scalable prior authorizations solution that embeds all Patient Health Information (PHI) in layers of security that is Electronic Data Interchange (EDI) compliant and stores the data on the cloud using 64-bit and 256-bit encryption that guarantees 100% HIPAA compliance.15,16
A Comprehensive and an Augmented Intelligence Solution to the Inevitable Prior Authorization Follow-Up, Appeals, and Changes Cloud-Based Solution
No longer relying on manual workflow, prior authorizations can be tracked using real-time analytics, followed up electronically 24/7, with the status continually updated on an interactive dashboard. When appeals are needed, customized solutions can be defined, and the system can seamlessly execute their protocols. This eliminates the need for practice or group personnel to spend countless hours on hold or faxing information to the myriad insurance payers, each with their own set of guidelines.
When unexpected changes are reported, including procedure level, service level, or demographics, the information is critical to the prior authorization process. With an augmented intelligence solution, unexpected changes can be accommodated and retransmitted in near real-time directly to the insurance payer without delay.
A Shifting Paradigm — Augmented Intelligence
By itself, automation and AI-driven software is capable of doing amazing things. However, to have a truly comprehensive prior authorization workflow, one must have a support team of experienced specialists with human intelligence and problem-solving skills. When emergent or complex requests and exceptions arise, it will be through a team of trained specialists that an organization is ensured complete coverage for their prior authorization process.
Moving forward following the pandemic, providers are finding themselves with challenges, both financial and carerelated. By taking advantage of advanced technology coupled with targeted human intelligence, we are entering a new phase of proactive revenue generation and collection less reliant on slow antiquated systems and insurance limitations and more on resilience and purposefulness.
Lastly, the human component is required to make the decisions robotic automation and AI cannot. Only people with empathy and knowledge of each unique situation can tailor a patient’s experience to their context and needs. Those practices seeking completely automated solutions for prior authorization should instead look to a solution that does not remove the human intelligence factor. Many general-purpose AI solutions are nothing more than spot analytics solutions branded as AI, which require significant investments with uncertain results. Someday, AI may evolve to the point of completely automating the prior authorization process – but, until that day, practices should look to incorporate human intelligence for better decision making and outcomes.
Thanks for reading. If you’d like to see the footnotes, please download this white paper as a pdf here.
About Infinx
Infinx provides innovative and scalable payment lifecycle solutions for healthcare practices. Combining an intelligent, cloud-based platform driven by artificial intelligence and automation, with our trained and certified prior authorization, coding and billing specialists, we help clients realize revenue, enabling them to shift focus from administrative details to billable patient care.