The challenge of incomplete eligibility and benefits responses have long plagued patient access teams. Our latest Patient Access Plus product update tackles the challenge of incomplete benefits data head-on.
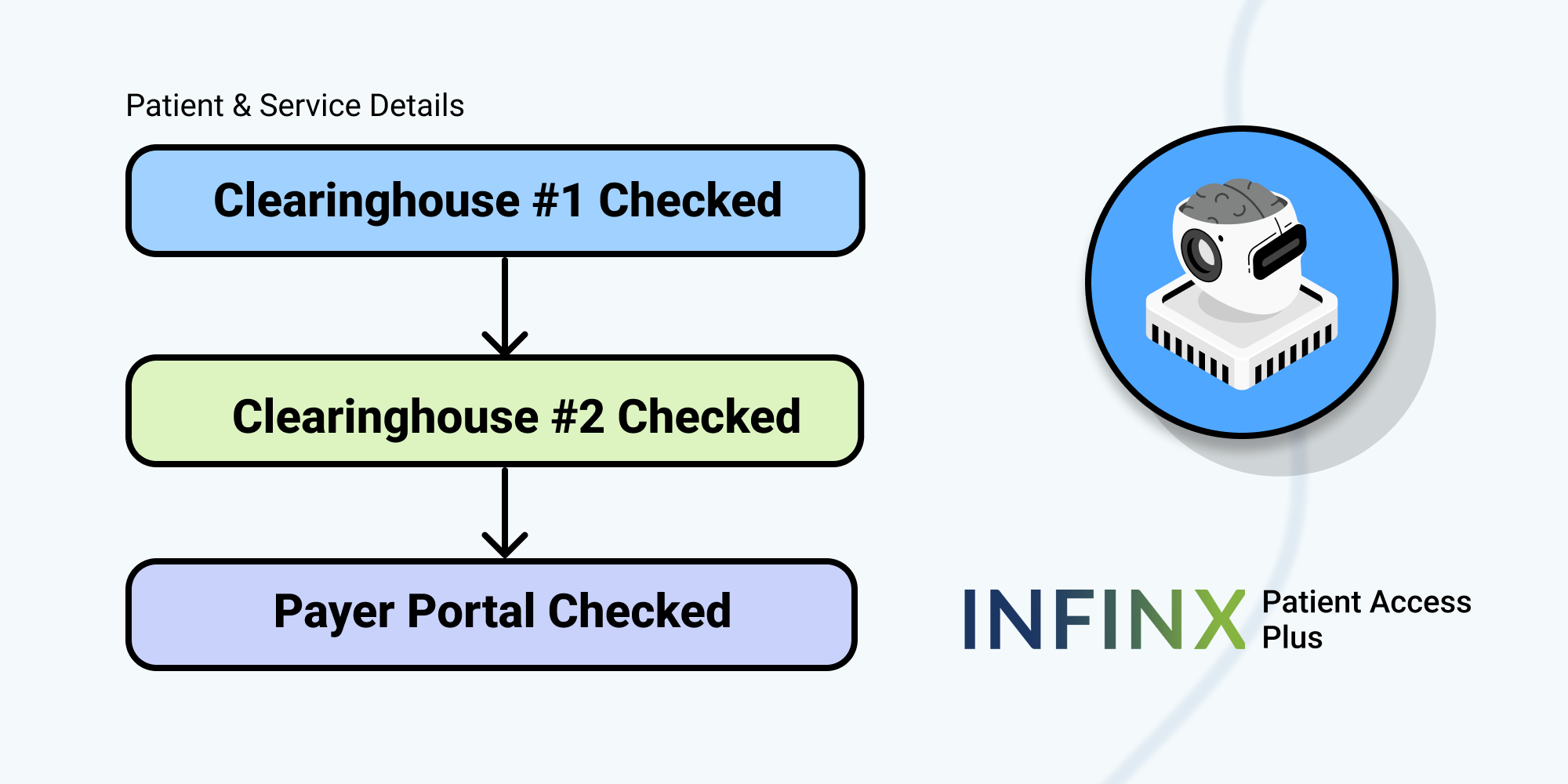
By integrating with multiple clearinghouses and payer portals, we ensure no detail is missed. If we receive partial data from one source, our platform dynamically pivots to another source, cascading through our clearinghouse connections and leveraging our proprietary payer portal automations to fill in the gaps. This approach ensures that we cover a 98-99% of payers, provide comprehensive and accurate information, and automate out as much manual work as possible.
With our enhanced benefits extraction algorithms, we don’t just collect data – we curate it, providing you with precise, service-level benefits information so you can schedule patients with confidence.
Whether it’s standard benefits information or more specific needs like authorization requirements, our system is equipped to handle it per your requirements.
And in the case where information is still missing, we’ve got you covered – we’ll either call and get it from the payer on your behalf or flag it for your team’s attention.
If you are looking to get curated benefits checks in real-time, please schedule a demo to see how we can help.
For more information on our Patient Access Plus Eligibility & Benefits Verification platform, click here to learn more.