With the Centers for Medicare and Medicaid Services (CMS) extending the mandatory implementation date to January 1, 2022, radiology practices, outpatient imaging centers, and hospital facilities continue to weigh their readiness to implement the systems necessary for compliance with the CMS Medicare rules governing the Appropriate Use Criteria (AUC) Program. This is part of the “Protecting Access to Medicare Act” (PAMA) passed by Congress in 2014 and is designed to improve diagnostic accuracy and quality of care while reducing unnecessary testing for Medicare patients.
With respect to Radiology, the AUC Program is focused on supporting referring providers when ordering advanced diagnostic imaging services to include MRI, CT, Nuclear Medicine, and PET. It’s mandated that when ordering these advanced imaging services, the referring provider or their designee will be required to consult a Clinical Decision Support Mechanism (CDSM), an interactive, electronic portal where they can access AUC that will greatly enhance the clinical decision experience.
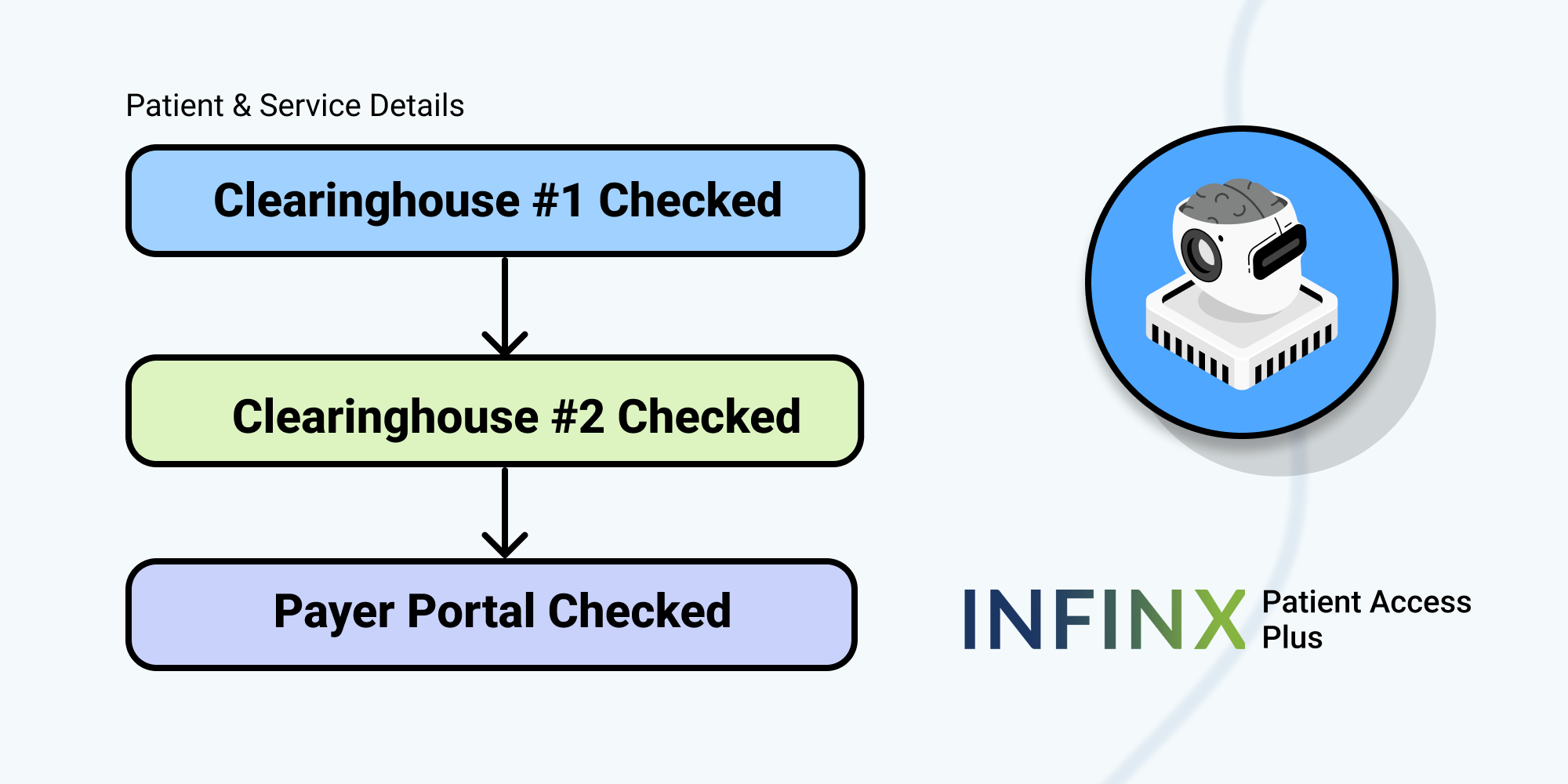
CMS has an approved list of vendors, of which Infinx is a participating member, that can provide the advanced automation to process certificates of compliance for CDSM that will ensure payment from Medicare after the mandatory implementation date of January 1, 2022 Certificates of compliance can be initiated by your group reactively if the patient is referred without the appropriate CDSM approval.
CDSM and Radiology Practices
Looking through the radiology lens, the AUC Program and CDSM were conceived as a process that would complement and elevate the referring provider’s diagnostic practice, strengthen the Medicare patient experience, and reduce needless advanced image testing. The requirement impacts all physicians, APP, and facilities billing Part B Services to Medicare. Note that exclusions are being made for emergency patient encounters, inpatient services billed through Part A, and ordering professionals with significant hardship, such as technological constraints or no access to internet services.
Whether seeking a modular system that integrates with existing prior approval software or a stand-alone CDSM package from the CMS published list of approved vendors, consider a partner that offers these valuable components:
- A comprehensive and up-to-date library of AUC’s sourced from multiple Qualified Provider Lead Entities (qPLE’s)
- A clinical dashboard that provides immediate access to current patient information for both furnishing and ordering physicians
- Coverage of all priority clinical areas as detailed by the CMS, including coronary artery disease (suspected or diagnosed), suspected pulmonary embolism, headache, hip pain, low back pain, shoulder pain (to include suspected rotator cuff injury), cancer of the lung (primary or metastatic, suspected or diagnosed)
- Ability to support referring providers within their EMR systems
- Ability to generate compliance certificates required for reimbursement
- Meets all security requirements and HIPAA compliance standards
Are Referring Providers Prepared?
The American College of Radiology (ACR) has recently noted the general consensus among contributing members is that referring providers are lacking awareness of the new program and are still unfamiliar or apprehensive of the deadline for implementation. As the furnishing professional, you have the financial stake in the outcome, and beginning January 1, 2022, claims submitted without compliance certificates will be rejected.
This has created a somewhat awkward situation that may best be resolved by radiologists partnering with their hospital colleagues to spearhead an awareness campaign that educates primary care providers in the benefits brought by AUC and CDSM. While this is currently mandated for Medicare patients only, be assured that third-party insurance carriers will have a keen eye on the roll-out and implementation in 2020.
Medicare Coding and Reimbursement for Radiology
The CMS has announced HCPCS G-codes to be used to modify the ICD-10 diagnosis codes. The “compliance certificate” then becomes part of the patient’s EHR and must be transmitted to the referring provider to supplement their billing and claim submission process.
At face value, the new requirements seem overly burdensome, but it will provide valuable data to help demonstrate utilization management as future healthcare criteria evolve through the CMS. AUC and CDSM can ultimately reduce the administrative burden on imaging providers and significantly strengthen the patient experience.
Ultimately, the best way to ease the operational requirements may be to consider a Software-as-a-Service (SaaS) solution that integrates into a component such as the Infinx Prior Authorization Software. This would provide immediate access to both referring/ordering and rendering providers, alleviating some of the administrative burdens.
Contact Infinx for more information about how the Infinx CDSM Solution can help you become compliant and ensure Medicare reimbursement.