One of the toughest choices, when faced with aging AR, is where to focus energy to get the maximum bang for your buck! Is it “all hands on deck” to work the denied claims report, or should everyone grab a phone and start dialing insurance companies to check the status on pending claims? It can feel overwhelming and is often not addressed until it’s at the crisis stage.
But what if today’s advances in technology created solutions that allowed you to address the age-old AR problem and effectively streamline the process to recover and capture revenue that might have been abandoned in the past? Not only would this bring more money to the bottom line, but it could also free up staff to focus more intently on the patient experience?
How Automation Can Improve AR Recovery in Cardiology
Accepted as part of the process, insurance payers add additional layers to AR management that create complicated and time-consuming follow-up, often limited by arbitrary rules and regulations. According to the 2019 CAQH Index, only about 70% of practices are using some or partial automation when it comes to checking claims status.
For the rest, that means only a certain number of claim statuses can be checked during each individual call to each specific payer—once that limit has been reached, the caller must hang up and call again, often waiting on hold for extended periods of time. While this may afford everyone a fair opportunity to get their claim status checked, it creates frustration for administrative staff and often causes claims to go stagnant.
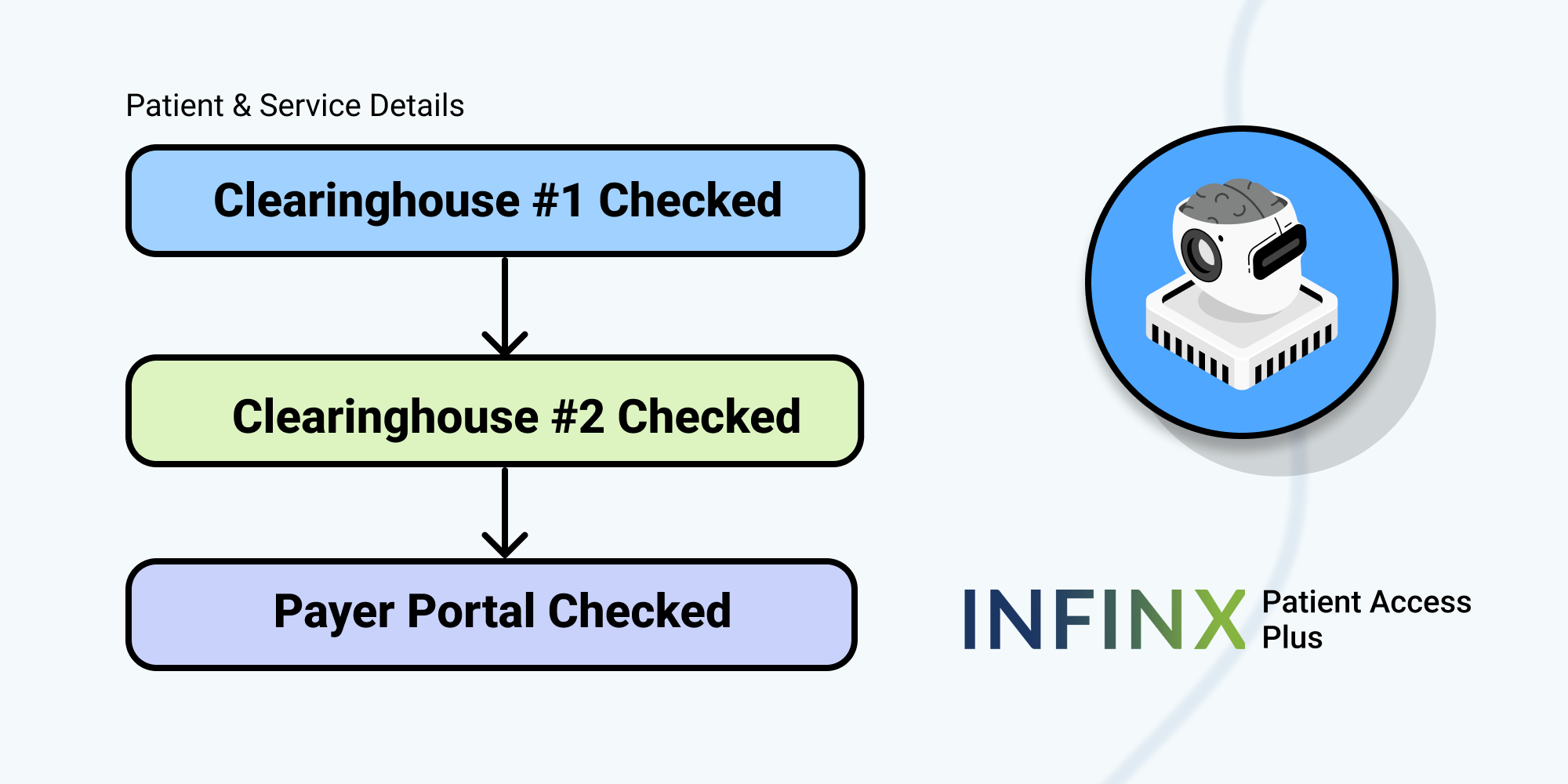
By utilizing an AR optimization solution in partnership with a third-party team, your cardiology practice would benefit from advanced automation using AI-driven software. Coupled with your patient insurance, demographic, and care information, this type of automated system would be able to access a vast clearinghouse of insurance payer information and then:
- Determine the next best course of action based on predictive insight algorithms that would examine and categorize multiple data points to expedite payments and reduce denials.
- Automate the follow-up process to prioritize and capture every possible dollar, including monitoring timely filing limits and payer guidelines specific to each insurance carrier.
- Provide accurate forecasts of potential collectible dollars to eliminate guessing and identify risks on in-process claims for predicted recovery.
- Examine claims data to provide overall analytics and guide best practice improvements throughout the patient access and billing processes that could improve everything from coding to the prior authorizations process.
- All of this supported by highly-experienced technicians focused on maximizing every claim and collecting every dollar due to your practice.
- Through an Insurance Discovery module, your practice would be able to scour clearinghouses and insurance payer databases to obtain undisclosed insurance coverage for patients that can then correct and resubmit claims and head off the collections process.
By taking charge of your A/R recovery program with the help of a third-party partner using AI-driven software, your practice could recognize an increase in collected revenue, a reduction in the number of denied claims, and an appeals process that is timely and effective. Also, by obtaining a blueprint of possible improvements through data analytics, you would obtain an operational view that could bring further efficiencies throughout the entire practice to ensure its continued growth and solvency into the new decade.
Take our quiz specifically for Cardiology practices to find out what’s blocking your practice from recognizing the maximum revenue.
Contact us to learn more about AR Optimization Solution using automation and AI-driven software to increase your revenue.