Below is our recent interview with Jaideep Tandon, Co-Founder of Infinx Healthcare:
Q: Could you provide our readers with a brief introduction to Infinx Healthcare?
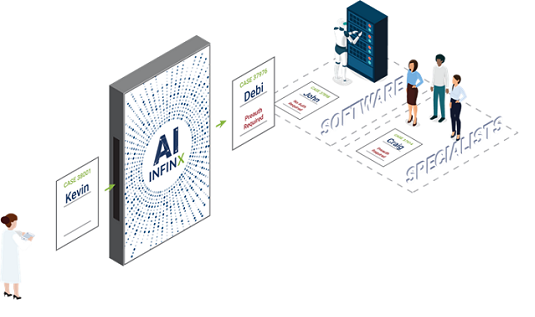
A: Sure. In short, Infinx provides intelligent payment lifecycle solutions for healthcare providers for multiple specialties. We offer a host of innovative solutions from our AI-powered prior authorization and denials management software to medical coding and billing support by our certified specialists.
Q: You’ve recently unveiled a new prior authorization determination engine; could you tell us something more?
A: Absolutely, It’s a deterministic rules-based engine built using machine learning models that automates the determination process of prior authorization and provides customers with a real-time answer to whether or not a prior authorization is required or not.
This new prior authorization determination engine is part of our Patient Access software, which leverages AI to analyze the client’s data and provide deep insight into their prior authorization process.
The determination engine is just the beginning. We are also poised to release a number of new features including a Turn Around Time Estimator, which can predict how long a prior authorization will take to be obtained; Risk Insights, which will be able to identify a prior authorization of having a high risk of denial; and a Medical Necessity Evaluator, which will analyze a case and determine if it fulfills medical necessity.
We understand that prior authorization cannot be 100% automated. While prior authorization cannot be 100% automated, certain aspects of the prior authorization process, such as interpreting handwritten notes on a report and handling approval for complicated procedures, will probably always require the human touch, Infinx is on a mission to automate as much of the prior authorization process as possible.
Recommended: Thomas Suter, CEO QCAM Currency Asset Management: We Support Clients In Harnessing Untapped Potential In Currencies
Q: Can you give us insights into your solutions?
A: While we’re on a mission to automate as much of the prior authorization process as possible, we understand that prior authorization cannot be 100% automated. Complicated procedures and payers who do not accept electronic submissions are handled by our prior authorization and billing specialists. This way, we offer a complete solution, versus kicking back the case for our client to process when more information is required.
Our software blends automation, integration, cognition, and control to provide an optimized workflow for the entire patient access process. With intuitive feature sets, we’re able to provide successful outcomes at each patient touch point. It also provides seamless HL7 integration to your EHR and a vast network of clearinghouse integrations.
The Patient Access software has three primary components:
1) It allows clients to automate 100 percent of their insurance verification and eligibility requests, which results in increased payment velocity and moves you from coverage unknowns to insurance verification in seconds;
2) It provides real-time patient pay data for all of your patient cases, which increases the patient’s understanding of payment responsibility and provides clients with payment certainty;
3) Prior authorizations are streamlined for real-time decision making on scheduling patients, and reducing medical necessity concerns. The case view provides detailed information on when a prior authorization will be completed. Exception cases that cannot be automated are managed by our team of trained specialists who have deep knowledge of payer guidelines and protocols.

Recommended: An Interview With Ray Marshall, CEO Of mSecure Password Manager
Q: How exactly do you help your clients preserve and capture more revenue?
A: Prior authorizations alone represent billions of dollars of missed revenue and millions of lost hours in productivity by physicians and staff. The burden of prior authorization is overwhelming for U.S. physicians and staff. It’s been estimated that the average physician spends an average of 20 hours per week and nearly $83,000 per year interacting with insurance plans and fixing prior authorization issues. In a regulatory landscape that is only going to demand more time-consuming bureaucracy, not less, it is a liability to not contract with a third party to help ensure you get paid. We hate to use the phrase no-brainer, but it’s a no-brainer.
There are numerous prior authorization and revenue cycle management processes steadily leak revenue without a dedicated solution in place. That’s where Infinx comes in.
We help healthcare providers preserve revenue before the appointment with our software plus specialists solution by ensuring that the patient has insurance and the procedure they are about to perform is authorized by insurance. We also help maximize revenue post-appointment by helping providers submit clean claims to payers and ensure that they get paid on time.
Q: What are your plans for the future?
A: Infinx intends to remain at the forefront of the healthcare industry’s automation revolution. We want to continue to make it more cost-effective for healthcare providers to run day-to-day operations and provide both patients and physician’s transparency and real-time analytics to achieve the greatest possible outcome for everyone involved.