Foundationally, the entire patient access process supports timely and accurate reimbursement from insurance payers — and insurance verification is one of the main components. If you operate in the complex and unique world of healthcare revenue cycle management (RCM), then you understand that verifying a patient’s eligibility is paramount in collecting the revenue you are generating.
While insurance verification was historically a slow and arduous process that included phone calls with lengthy hold times and rejected claims due to missing or inaccurate information, today’s advanced technology allows you to check insurance in real-time.
Not Everyone Has Caught On
While many healthcare providers have implemented an automated insurance verification process (over 84% according to the 2019 CAQH Index on Conducting Electronic Business Transactions), many have still not. And of those using digital insurance verification, many are not using it to its fullest potential.
In fact, the CAQH Index notes that converting from a manual system to a fully electronic insurance verification and benefit eligibility process would save $4.12 per patient and go from costing $5.30 per instance to just $1.18.
Consider Improving Your Patient Assimilation
Whether your hospital department or practice provides appointment scheduling with a live person, a call center, or a patient portal, this is usually the first opportunity to set the tone with your new patient regarding the expectations to follow in terms of RCM.
Initial Point of Contact: Appointment Scheduling and Demographics Collection
Collect accurate insurance information, including current demographics, before the patient is even scheduled. This ensures that the patient is eligible to receive treatment at the contracted rates indicated by their plan.
Insurance should be verified each time you encounter the patient — scheduling phone calls, arrival/check-in, follow-up appointments, etc. This is the only way to ensure valid RCM information is ongoing and current for the following:
- Insurance eligibility dates
- Co-pays and co-insurances
- Deductibles
- Secondary insurance and coordination of benefits
- In-network vs. out-of-network coverage
- Referral requirements
- Prior authorization requirements
Remember, there is another important process during this initial scheduling phase — educating the patient on financial policies and payment expectations, missed appointment charges, and cancellation policies. You will have other opportunities to reinforce your financial guidelines as the relationship develops but starting with a strong foundation will certainly help down the road.
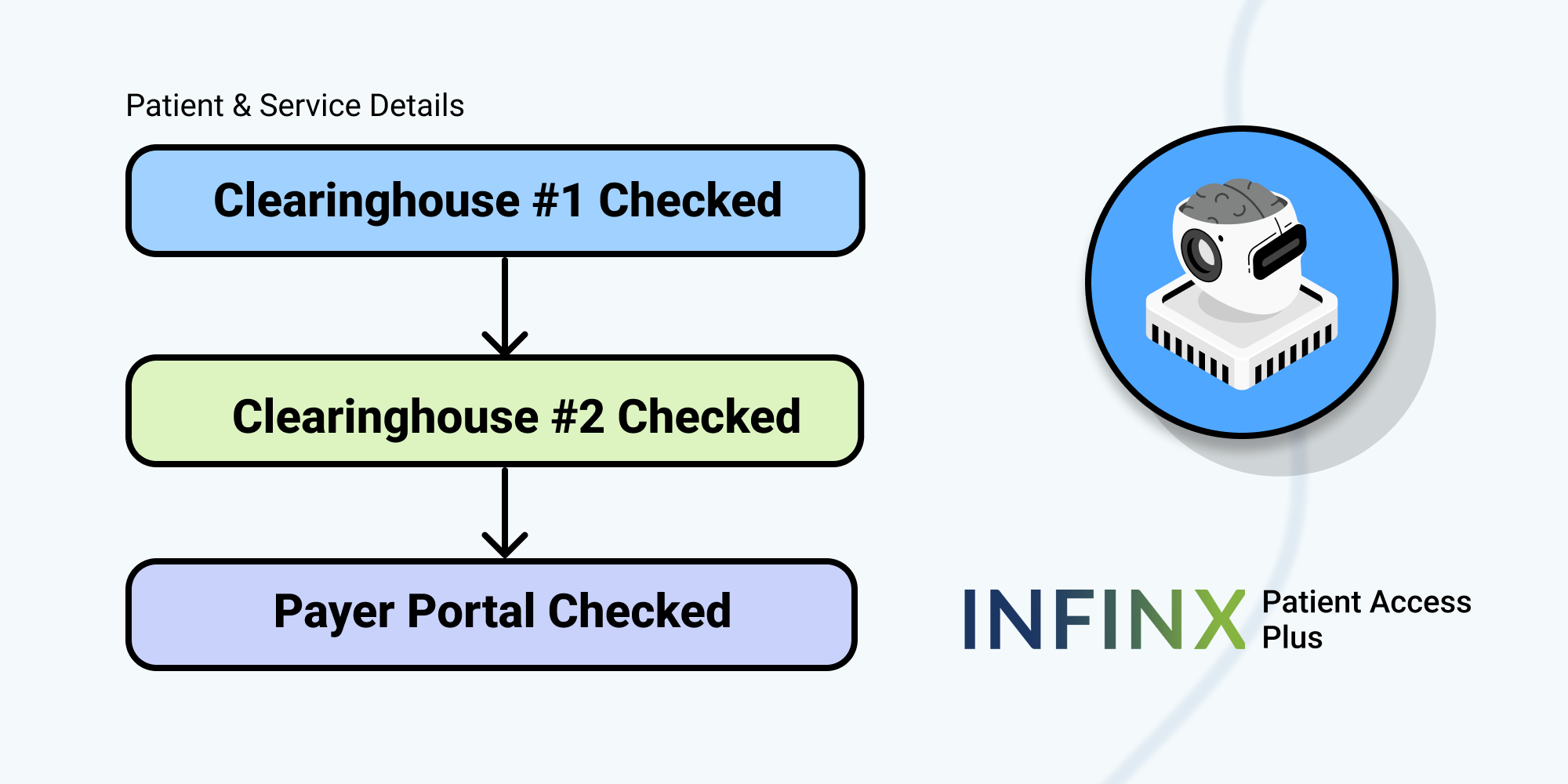
Using a fully automated insurance verification process, patient information can be checked or double-checked in real-time without placing an undue burden on the business office staff. Your entire RCM process should proceed more smoothly with fewer denied claims and less follow-up and re-submission of corrected claims.
Once you have secured the insurance verification process, the next step is to formalize a patient portion due collection system where estimated amounts are collected before the initial visit.
Patient Pay Estimation and Collection Ahead of Service
Today, fully 30% or more of the cost of healthcare may be the patient’s responsibility – services you provide and should be compensated for – and the patient should be aware of this amount before entering your practice. While there are always unforeseen circumstances that arise, a large percentage of costs can be well researched and pinpointed ahead of the actual visit.
It has long been customary for many practices to notify patients of pending amounts due as they arrive, which is often a shock to the individual and sets up an adversarial relationship from the start. But what if you are proactive in notifying your patients about payments ahead of an appointment and requesting payment at that time?
This allows the patient to digest the amount, ask questions, research their insurance plan, and become an active participant in the process. It also encourages your staff to identify potential concerns and to offer arrangements that reinforce an obligation, such as 50% now-50% at the time of service or third-party financial plans.
To Sum Up
Paying special attention to the initial patient onboarding process, or patient access lays a healthy foundation for the ongoing relationship you will have with a patient. It’s better to be upfront with expectations — this builds trust with the patient and removes any potential problems before they occur.
Contact us to discuss our Insurance Verification & Benefits module, part of our Prior Authorization Software.