In today’s complex healthcare market, radiology practices are challenged with increasing regulations and governmental oversight, declining fee schedules and changing reimbursement parameters. Once the patient has been seen, and the best care delivered, ensuring accurate, fast reimbursement becomes of paramount importance. And unique to radiology, which may include the technical component or the professional component — or both.
Have You Taken an Unbiased View of the Process?
Examining the system that is in place with a fresh pair of eyes will often lead to innovative ideas and bold changes that will help the flow and increase the amount and speed of collections. The first question to ask is “are we using the best automation available within our budget”?
Technology is continually changing and evolving in the radiology field when it comes to diagnostic and treatment tools; it moves at an equally fast pace when it comes to the patient’s financial experience. Once you are comfortable that you have the best tools in place, then challenge your business office to look objectively at how they accomplish their jobs and if some changes or improvements that would streamline the process for everyone.
5 Ideas that are Often Overlooked
-
Stay Current on Coding Changes — While the bulk of coding changes are usually announced in the final quarter of the previous year with an effective date of January 1st, information can change throughout the year. A good example has been the telehealth changes that impacted patient E/M codes and ICD-10-CM codes during the COVID-19 pandemic.
Another example are the modifiers that were released mid-year 2019 that are used for Medicare patients impacted by Appropriate Use Criteria (AUC):
- Modifier MA – The ordering professional is not required to check with a Clinical Decision Support Mechanism (CDSM) because a service is being rendered to the patient with a confirmed or suspected emergency medical problem.
- Modifier MB – Due to significant hardship of internet access that is insufficient, the ordering professional is not required to produce a compliance certificate through CDSM.
- Modifier ME – The order for the service meets the appropriate use criteria and was provided by a CDSM, which was consulted by the ordering provider.
- Modifier MF – The ordering professional consulted the CDSM, but the order for services is counter to the AUC.
- Modifier MG – There isn’t an AUC for the ordered service within the CDSM, which the ordering professional consulted.
- Modifier MH – It is unknown whether the ordering provider consulted the CDSM; and related information not provided to the furnishing provider or professional.
-
Review Templates for Documentation Needs — Many EHR/EMR/RISs have templates used for documentation. However, these templates should be reviewed at least annually to ensure that the layout and flow are appropriate and that the documentation fits with changes to billing requirements.
-
Ensure Clinical Decision Support Mechanism Compliance — This year saw the start of the CDSM testing phase impacting all Medicare patients. It’s important that this system is working before 2022 where mandatory consequences will negate or disallow reimbursement due to missing compliance certificates. It’s also good to double-check with your ordering provider base to make sure that they have no roadblocks to your practice or ordering your services.
Special Note: The CMS recently updated the mandatory implementation date from January 1, 2021, to January 1, 2022, recognizing the complexity of the program required additional time for training and technological workflow challenges.
-
Begin the Collections Process During Patient Scheduling — As patient responsibility has grown over the last number of years, so have problems that come from “surprise billings” and growing collections. By restructuring the patient onboarding process to include collecting for any portions due prior to treatment scheduling, revenue that used to end up in the AR and collections is actually accounted for upfront.
This not only improves the bottom line with fewer accounts going to collections or becoming uncollectible but improves the patient’s experience by offering an honest discussion at the beginning and no “surprises” later.
-
Leverage Technology for Maximum AR Optimization — Once a claim is denied, it requires some change or adjustment to resubmit. Unfortunately, according to the Medical Group Management Association (MGMA), 50 to 65% of denials are never processed due to a lack of time or understanding of the mechanics. Additionally, the cost to reprocess with a mostly manual system is $25 per claim. This potentially leaves significant revenue on the table to be forfeited.
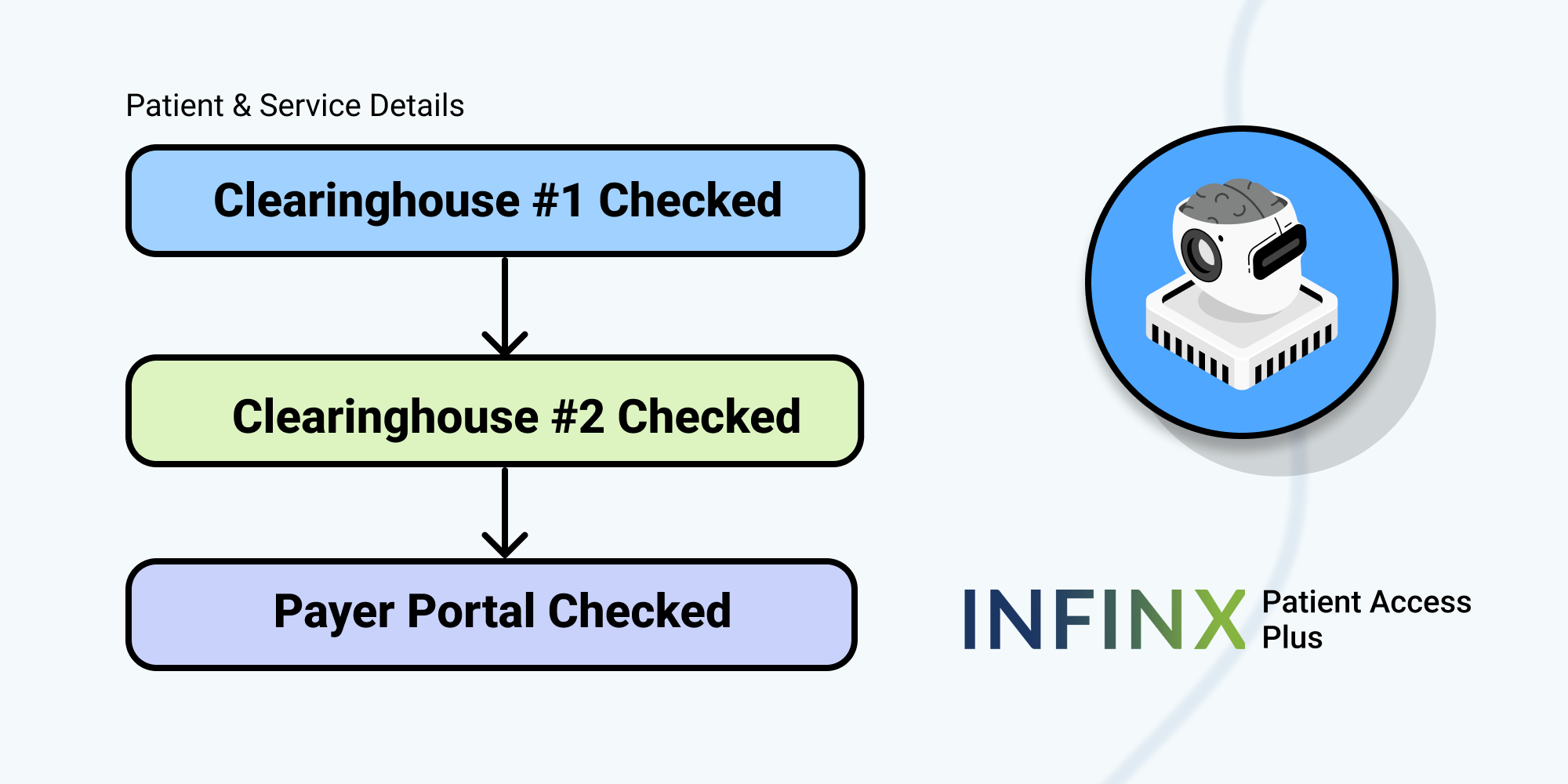
By leveraging advanced technology to optimize your outstanding ARs, an AI-driven software with machine learning capabilities can determine collectability and guide efforts where needed. Additionally, by using a tech-enabled system, expert specialists are supporting the full AR process.
Radiology groups are unique with multiple types of facilities and inpatient vs. outpatient opportunities. Whatever the mix, ensuring a strong revenue cycle management process will help create success in the ultra-complex third-party payer system that we have in healthcare. Whether committed to in-house or outsourced partners, the billing team is critical to the bottom-line.
Contact us to learn about efficient, streamlined radiology billing to improve your bottom-line.